Preserving Organ: A Beacon of Hope for Improved Life
- Published Date: September 15, 2023
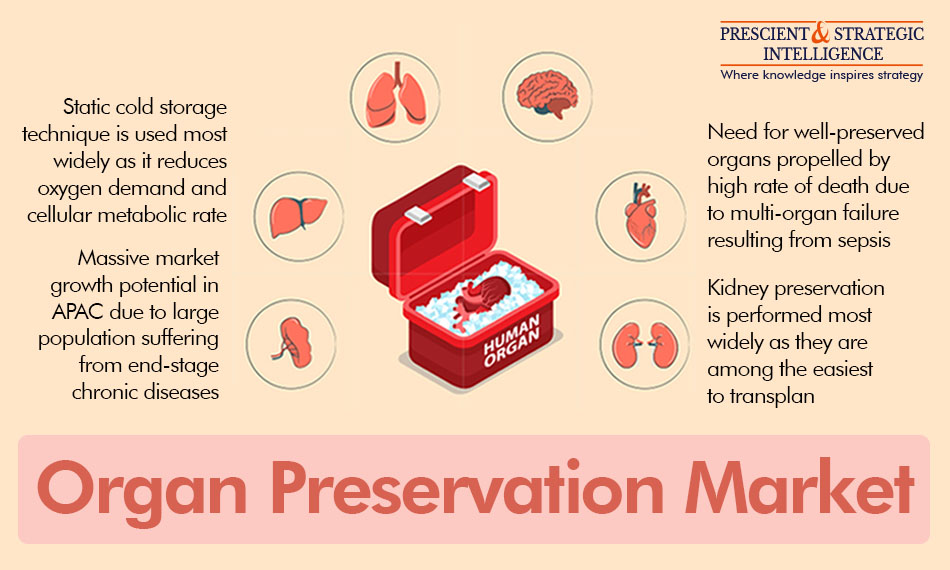
Organ preservation is one of the most-important fields in medicine that concentrates on preserving the feasibility and functionality of organs outside the human body, for transplanting, study, and numerous other purposes. Recent advances in preserving technologies have transformed the world of organ transplantation, offering an enormous potential to patients to live a normal life.
One of the major purposes of preserving an organ is to lengthen its life, permitting it to be delivered from donors to patients over lengthier distances and increasing the odds of a successful transplant. The old-style approach of accomplishing the purpose involved easy cold storage, where the organs were held in the freezer at a rather low temperature, to delay cellular metabolism and decrease damage.
Recent developments in organ preservation methods have led to more-urbane approaches. For example, hypothermic machine perfusion involves passing a cold, protective solution through the organ, offering improved preservation outcomes in comparison to static cold storage. This method supports in maintaining organ function, decreases tissue impairment, and increases the possibility of a successful transplant.
The preservation of organs is not restricted to transplantation only. It also plays an important role in clinical studies, medication testing, and the development of regenerative drugs. Furthermore, the rise of biotechnology and tissue engineering has unlocked doors for the growth of artificial tissues and organs.
History of Organ Preservation
The past of organ preservation is marked by substantial improvements in medicinal science. At the beginning of the 20th century, the transplantation of an organ was restricted due to a lack of effective technologies for its preservation outside the body. In 1954, the first successful kidney transplant took place, but still, preservation of an organ remained a challenge.
In the 1960s, the development of hypothermic preservation solutions, such as the University of Wisconsin solution, revolutionized the field. These solutions allow organs to be stored at low temperatures, thus slowing metabolic processes and extending their viability. This breakthrough has enabled the successful transplantation of various organs, including the heart and liver.
Further, in the 1980s, the emergence of machine perfusion changed the game. It is a method where the organs are held in a working order and nurtured by a pumping machine. This advanced conservation technique decreases the danger of harm to tissues due to ischemia and augments organ viability.
Types of Solutions Used for Organ Preservation
For organ preservation, numerous kinds of solutions are utilized, all of which are made to preserve them long enough to be transported and transplanted. Here are some popular types:
University of Wisconsin Solution: The UW solution is a hyperosmolar solution that stops the swelling of cells, upholds steady transmembrane electrochemical gradient upon reperfusion, by averting the loss of intracellular potassium throughout storage; and comprises a range of oxygen-free radical hunters.
Custodiol HTK Solution: Custodiol HTK is also used for cold storage. It contains numerous antioxidants and electrolytes to maintain the organ's metabolic working during preservation. The solution, which contains histidine, tryptophan, and ketoglutarate, is progressively being utilized for the kidneys and livers. Tryptophan acts as an antioxidant and membrane additive, while ketoglutarate serves as a substratum for anaerobiotic metabolism during preservation.
Perfluorocarbon Solution: This oxygen-carrying agent can be utilized to flush and preserve organs. As it does not bind oxygen, the gas can be better released to the surrounding tissue than hemoglobin.
Collins/Euro-Collins Solution: The Collins solution contains high amounts of potassium and low concentrations of sodium, along with phosphate buffers and glucose. European scientists modified this solution by increasing the concentration of glucose from 140 mmol per liter to 195 mmol per liter.
The Process of Organ Preservation
Prior to being detached from the donor, every organ is cleaned and made free of blood with a special ice-cold conservation solution that comprises nutrients and electrolytes. The organs are then shifted to germ-free ampules, packed in wet ice, and transported to the patient's hospital. It is vital to ferry organs from the benefactor to the recipient as fast as possible. The lungs and hearts should be transplanted within 4 hours after being detached from the donor. The liver can be conserved for 12–18 hours; a pancreas can be conserved for 10–12 hours; the intestines are viable for around 8 hours; while the kidneys can be transplanted 24–36 hours after extraction.
Importance of Organ Donation
Organ donation is extremely important as it can save many lives. According to the Health Resources & Services Administration, 104,234 men, women, and children are on the national transplant waiting list in the U.S. Every day, around 17 people die waiting for an organ. Each donor has the potential to save eight lives and enhance over 75 more. In 2022, around 42,000 transplants were performed, with another person added to the transplant waiting list every 10 minutes.
These disheartening statistics result from the huge gap in the availability of viable organs relative to the demand. This is itself because of both a lack of willing donors as well as the lax standards followed in many parts of the world during organ extraction, preservation, and transportation. Therefore, nations must consider effective strategies to meet the rising demand for transplantable organs.
Several people have said that a shift from an “opt-in” to an “opt-out” rule for organ donation will significantly improve donor counts. An opt-out rule assumes that each individual is aware of the importance of organs for saving lives and they are willing to be a donor after their death. Those who are not in favor of donating are required to make this clear, typically by writing an official declaration to this effect.
Commonly, the first reaction of people to opt out of actively signing up for donating their vital body parts is that it is a good plan as there are millions of people who are in need of organs. However, changing to an opt-out system is not this simple, primarily because of the ethical concerns revolving around the rights of a person on their body after their death.
Role of Efficient Transportation in Organ Preservation
Transportation plays a vital role in transplantation by guaranteeing the fastest possible delivery of organs from donors to patients. A quick transport is imperative because of the inability of organs and tissues to survive for long outside their natural environment, meaning the donor’s body. Here are a few major aspects of its importance:
Time Sensitivity: Human organs have a restricted cold ischemia period, in which they can stay feasible outside the human body. Transportation should be smooth to minimize this period and increase the probability of a successful transplant.
Patient Lives: A rapid transport protects lives by offering critically ill patients the organs they require. Any interruptions in the transport in this situation can result in organ harm or make transplantation tough and the post-operative period full of risks for the recipient.
Coordination: Conveying organs needs careful preparation and communication between medicinal teams, donor infirmaries, and transplantation centers. Transport logistics are as essential as surgical expertise, with the cold chain constituting a major aspect of the whole process.
Medical Equipment: Dedicated transportation containers and machines preserve organs at the needed temperature and circumstances, to prevent any harm.
Success Rates: Well-organized transportation results in higher success rates for organ transplants, guaranteeing that more patients obtain the gift of life.
Importance of Preserving an Organ Well
If organs are not well-preserved for transplantation, there is a possibility of serious health problems or even the death of the recipient. This is because of the extremely short cold ischemia period of most organs and the manifold risks not preserving them well can have for patients, their families, doctors and the healthcare system, and the society at large.
Organ Failure: If an organ is not preserved or poorly persevered and transplanted into a patient, then there is a high possibility that it will not work as expected. In extreme cases, this leads to organ failure. This can be life-threatening and might need transplantation again, which is not easy because of a lack of organ donors and the exorbitant costs involved.
Increased Surgical Risks: Transplant operations are difficult and carry inherent dangers. When organs are poorly preserved, the operation becomes more complex and dangerous, with an increased possibility of demise during or after it.
Infection and Sepsis: Improperly conserved organs can be polluted by fungi, viruses, or bacteria, which can cause contagions in the patient. If such infections develop into sepsis, it can prove fatal.
Immune Rejection: Inefficient organ conservation can stimulate a tougher immune response in the patient, raising the danger of organ refusal by the body. If the body does not accept the organ, then it might need stronger immunosuppression than normal. This condition can become fatal if not handled properly.
Delayed Transplantation: If the organs are not preserved well, they might not fulfill the required standards for the transplant, thus leading to interruptions in discovering a match. For patients in a crucial need of transplants, such delays can be deadly.
Recent Developments in the Field of Organ Preservation
- In 2021, Paragonix Technologies introduced the LIVERguard organ preservation system in Europe and the U.S. It offers a carefully controlled environment for hypothermic liver preservation, along with enabling real-time digital monitoring.
- XVIVO Perfusion came into a cooperation with Contatori Medical in 2021 to offer its Liver Assist and Kidney Assist perfusion machines to transplantation centers in Brazil that have contracted Contatori Medical.
- In 2021, Institut Georges Lopez (Igl) (France) publicized plans to construct a facility in Cheyyar, Tamil Nadu, India, for creating equipment and solutions that will be used to flush and preserve of organs.
- In 2021, the Food and Drug Administration gave its the premarket approval to the OCS Heart System, developed by Transmedics, to be utilized with organs from donors after cardiac death.
- In 2020, Dr. Franz Khler Chemie GmbH, with the Melchers Group and CICEL GmbH, created Khler PharmaceuticalsBeijing Ltd. in China, for the supply of the Custodial HTK solution for heart transplants.
Promising Future of Organ Transplantation
Bioengineered Organs: Experts are studying the potential of making bioengineered organs in the laboratory. Such organs can be modified as per the patient's needs, thus decreasing the requirement for organ transplantation and the related danger of rejection by the body.
Organ Printing: 3D-printed organs can be utilized as and when the demand arises. This innovation has the potential to transform organ transplants by removing the requirement for donors, thus making transplants more accessible.
Improved Cryopreservation: Improvements in cryopreservation methods might ultimately make it possible to freeze and stock organs for a longer time, without cellular harm. This can dramatically increase the obtainability of organs for transplant.
Artificial Organs: The advent of artificial organs and machines that have the power to simulate the functioning of a real organ can give life-saving aid while patients wait for a donor match.
Nanotechnology: This technology could be utilized to advance organ conservation approaches by permitting a better screening and upkeep of organs during storage.
Organ on a Chip: The organ-on-a-chip technology, which duplicates the working and structure of organs on chips, is being utilized for testing the viability of organs before extracting, conserving, and transplanting them.
Gene Editing: Developments in gene editing, such as CRISPR-Cas9, can be utilized to alter donor organs, to make them a better match for patients, thus decreasing the danger of rejection.
AI and ML: These technologies can be used to forecast organ excellence and feasibility more precisely and aiding in matching them with the appropriate patient.
Conclusion
Organ conservation is an important field in medicine with a deep effect on transplants, examination, and the future of healthcare. In the past few decades, it has evolved from simple cold storage to cutting-edge methods, such as machine perfusion, which have enhanced the feasibility of organs and advanced patient outcomes.
By clicking the Send Message below, you also agree to abide by the Terms and Conditions of the company
We respect your privacy. Your information will not be shared.
